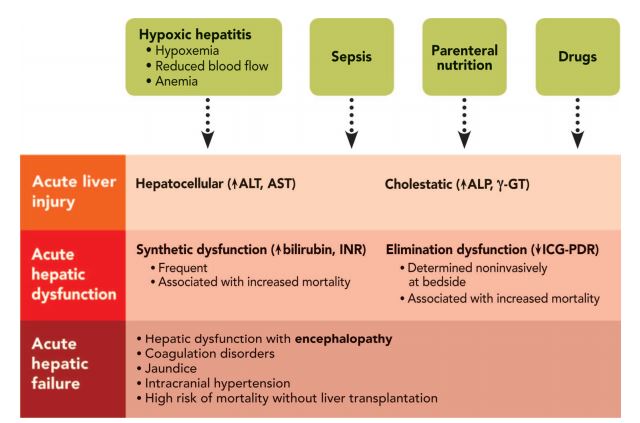
DEFINITIONS:
- liver injury – elevation in hepatic enzymes (ALT, AST, ALP, GGT)
- hepatic dysfunction – derangement of pathways related to synthetic or clearance function (INR and bilirubin)
- acute liver failure – liver injury that results in life-threatening hepatic synthetic dysfunction and brain dysfunction
HEPATOCELLULAR INJURY
- injury to hepatocystes
- elevation in serum aminotransferases
- duration of elevation depends on severity of insult and half-life of enzyme (17h for AST and 50h for ALT)
- most common causes
- hypoxic hepatitis
- congestive hepatopathy
- septic shock
- drug-induced
- AST is nonspecific, also produced in skeletal muscles, heart, lung, brain, kidney, pancreas, erythrocytes, leukocytes
- ALT is expressed mainly in the liver and normal levels exclude primary liver injury (EXCEPT in ETOH liver disease – deficiency in pyridoxal-5′-phosphate necessary for AST synthesis – low serum concentrations)
CHOLESTATIC INJURY
- altered bile production, secretion or excretion
- associated with increase in cholestatic enzymes s.a. ALP (very sensitive) and GGT, moderate or normal aminotransferases
HEPATIC DYSFUNCTION:
- bilirubin, albumin and INR
- causes of hyperbilirubinemia – increased production (hemolysis), decreased clearance (hepatic dysfunction) or decreased secretion (posthepatic occlusion, cholestasis)
- major causes in the ICU:
- insults leading to hepatocyte injury (ischemic)
- sepsis-associated cholestasis
- drug-induced liver injury
- parenteral nutrition
- serum and INR m albumin not specific for hepatic dysfunction in criticallyill
ELIMINATION FUNCTION
- some dynamic tests have been developed to assess functional capacityof the liver
- disappearance rate of teh colorant indocyanine green (ICG-PDF) to asses hepatic metabolic rate
- hepatic vein catheterization to measure hepatic vein oxygenation as marker of splanchnic ischemia
- measurement of liver stiffness by transient elastgraphy using Fibroscan instrument
MANAGEMENT OF ACUTE LIVER INJURY:
- Define the type of liver injury: hepatocelllular injury or cholestasis or mixed pattern
- perform microbiologic analysis and hepatic ultrasound
- maintain adequate arterial perfusion and fluid and electroiyte balances
- start early ABx in case of ongoing infection
- stop hepatotoxic medications
Causes of liver insults, definitions, and key points of intensive care unit (ICU) acquired acute liver injury, hepatic dysfunction, and acute liver failure.
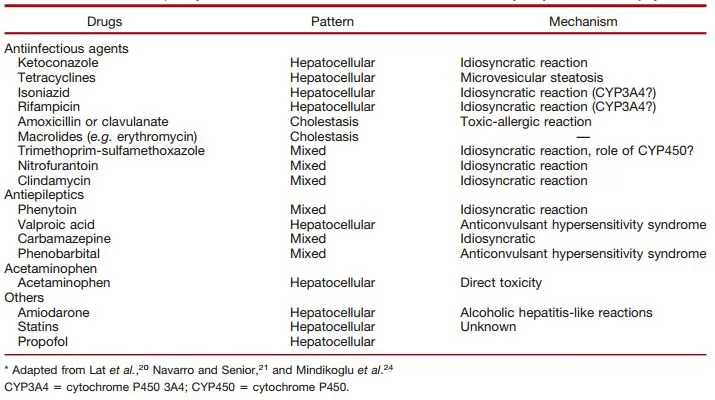
Medications Frequently Prescribed in the Intensive Care Unit that Potentially May Cause Liver Injury*
References
Lescot, Thomas et al. “Acquired Liver Injury In The Intensive Care Unit”. Anesthesiology 117.4 (2012): 898-904.